Atopic dermatitis, 30s female -Fecal microflora transplantation case report
Case presentation: 30s female, atopic dermatitis
summary
A patient with atopic dermatitis from childhood, exacerbated by stress, underwent six transplants over a period of about a month without immediate improvement. The patient’s condition improved dramatically 4 months after transplantation, following lifestyle modification and the addition of supplements. It suggests that depending on the patient’s condition, there may be a time lag between transplantation and symptom improvement.Basic Information
| Patients:. | 30’s Female |
| Attending physician:. | Luke’s Ashiya Clinic |
| Medical institution in charge of transplantation:. | Luke’s Ashiya Clinic |
Information at the time of initial medical examination
| Disease name:. | Atopic Dermatitis |
| At onset | 10 years ago |
| Transplant Purpose: To | skin problem |
| Chief complaint:. | He had been atopic since childhood, but 10 years ago he started working in the restaurant business, and his atopic condition worsened due to alcohol and stress. Since then, her condition has not improved even after she stopped drinking alcohol. She is currently raising two children (breastfeeding). |
| Medications being taken:. | Nerizona Cream Glimethasone |
| Medical history | Nothing |
| Background, family history, lifestyle, supplement use, etc.:. | He owned a bar for three years starting in his late 20s. During that time he drank every day. |
Transplant Information
| Transplantation period: from | June 27, 2018 – July 25, 2018 |
| Number of transplants | 6 times |
| Change from first transplant to end of transplant:. |
| 【2nd transplantation questionnaire】
He said: The day after the first one, my skin and stomach felt better, but the day after that, I felt like I was back again.
【3rd transplantation questionnaire】 She said: Since the second transplant, she had not had a bowel movement until yesterday. Skin is still itchy and I can’t sleep at night. From the doctor: intense redness on face, neck, and both hands. There is also exudate on hands. 【5th transplantation questionnaire】 The patient says: Skin symptoms remain the same, itchy and unable to sleep. Doctor’s note: Bilateral redness of fingers, face, and neck are also red. So far, there is no change in any other findings (bowel movements, mental health, etc.) except for the skin. 【6th transplantation questionnaire】 Patient’s story: Skin symptoms have not changed, and itching continues. Defecation is no longer muddy, but she has to have a bowel movement twice a week, which is uncomfortable and leaves her with a lingering sensation of having a stool. He feels that it was easier to have a bowel movement before. FROM THE DOCTOR: REDNESS OF FACE AND DORSUM OF HANDS IS INTENSE. ZINC DEFICIENCY, B-COMPLEX SUPPLEMENTS, BIOSLY, DIGESTIVE ENZYMES, AND ZINC PREPARATIONS STARTED. |
| Changes after completion of transplant:. |
| [September 2018]
His story: I’m done with the transplant, but it’s not getting any better. In fact, it’s getting worse. I’ve added Bioslee, but I don’t know if it’s working and I’m starting to get sick of it. I wonder if the transplant was really worth it. My bowel movements are worse than before and I only have them about twice a week.
From the doctor: Exacerbation of skin rash with exudate on fingers and neck. He is constantly scratching with itching.
[December 2018] He says: My skin condition is getting so much better. The itching is gone and I sleep better. I hardly use steroids. Stress is still there. I still have to take care of my children at night. Stress is still the same with my husband. From the physician: Redness on the face, neck, and extremities has decreased, and there is little desquamation. Her facial expression is bright. She has hardly taken any of the prescribed zinc medication. She is stressed, but the work we did in counseling to imagine “the place she loves most” is effective. She is now able to verbalize that she is happy to spend time with her child in her bedroom, which is a significant change. Zinc levels have always been low, and she continues to take a zinc preparation (Promax) to improve skin metabolism. |
Evaluation and Discussion
| Transplant Evaluation:. | Clear improvement of symptoms |
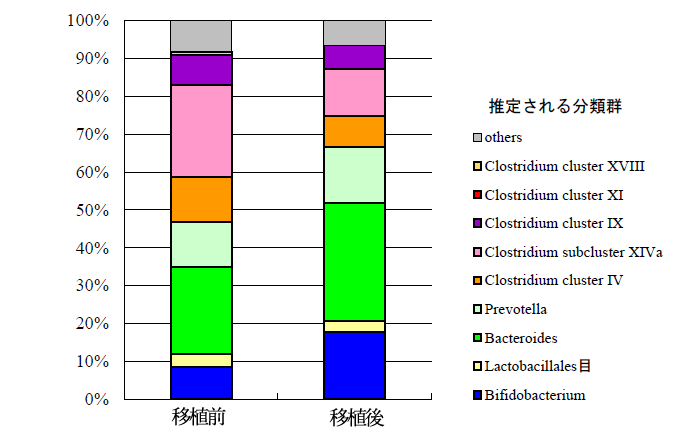
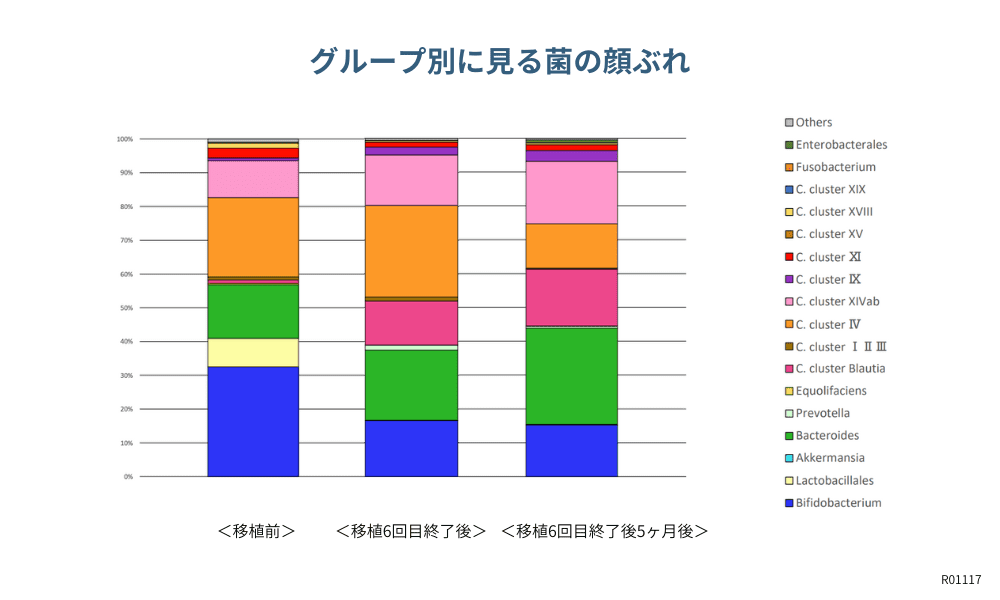
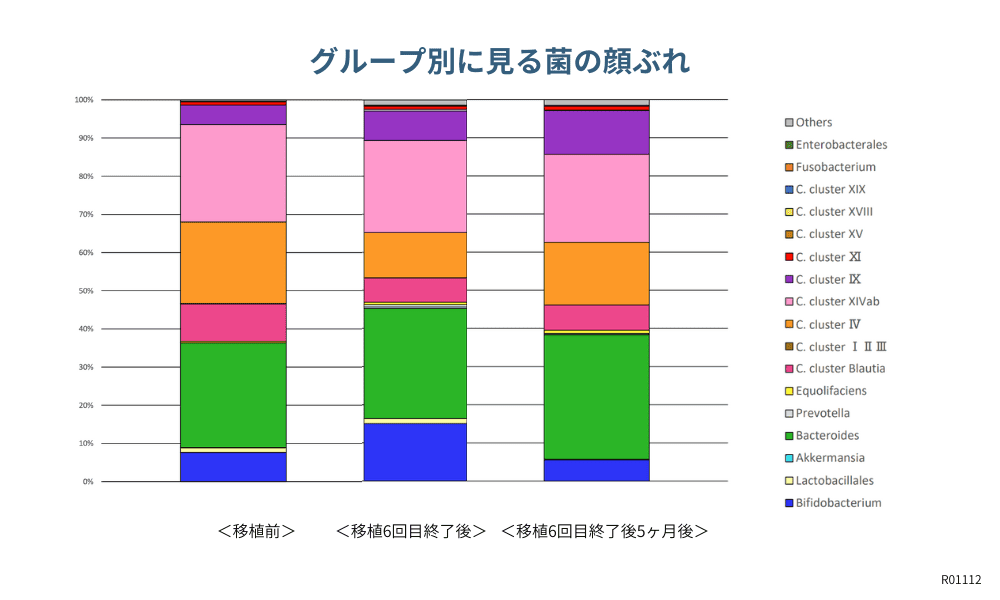
| Pre- and post-transplant flora balance test changes:. | [Before transplantation] June 2018.
As for the flora balance, the flora that mainly controls the mental aspect is particularly noticeably unbalanced. The overall bacterial diversity is fine, but it is assumed that Bacteroides and other bacteria pushed down by Clostridium spp. have been prevented from doing their good work as they should.
[After transplant] Implemented August 2018. The overall balance is greatly improved. In addition, the intestinal bacteria necessary to rebuild the skin are perfectly present, and we believe that the normalization of immune function and tissue rebuilding should catch up according to the metabolism of the intestinal bacteria. |
| Blood test changes:. | [After transplantation] None |
| POMS2 SCORE CHANGE:. | [After transplantation] None |
| His/her experience (from the questionnaire):. |
| Retrieved August 2018 Before transplant, expected to get better soon. No change during transplant. Immediately after transplant, I thought I had a slight improvement, but people around me said it got worse. |
| Adverse events: No |
| Yes (mild) Specific symptoms: Mild constipation Causal relationship with transplant: Probably related *Bowel movements gradually improved after transplant |
| Transplant General Comments and Discussion:. |
| Transplant General Comments and Discussion:. The improvement in the state of the intestinal microflora may be due to both the normalization of the function of Treg (regulatory T cells), which initiates intestinal immunity, and the regeneration of skin tissue by the function of the equol-producing strain. There have been several cases of atopic dermatitis and allergies that required several months to improve after transplantation, and the time required for improvement and the occurrence of minor adverse events due to a swing in immune function depend on the patient’s own age and immune function. In this case, we felt the need to take a long-term view of the patient’s treatment, such as supporting the patient to persevere even if symptoms do not change immediately after transplantation, and adding supplements as needed based on the results of blood tests and other tests. In addition, we would like to add that a psychological approach is also effective in treating atopic dermatitis, since a psychological aspect is often involved in the disease. |
Other
▼Photographs before transplantation
▼Photographs after transplantation
 … and upwards
… and upwards
Return to Top of Case Studies
その他の Intestinal flora transplantation and case studies に関する記事
Articles about other Intestinal flora transplantation and case studies
November 03, 2025
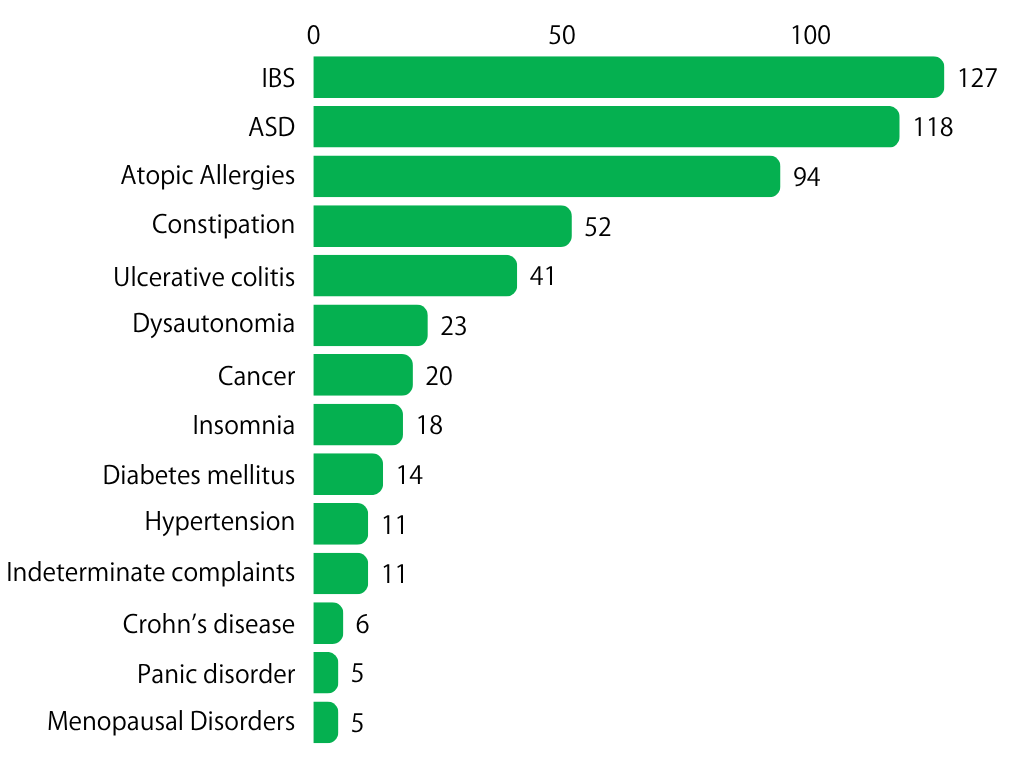
Fecal microbiota transplantation results *As of September , 2025
The number of actual fecal microbiota transplants by case in our study group is as follows Case reports by disease You can view case reports by disease from the links below: [Ulcerative Colitis]https://fmt-japan.org/research-activities/fmt-cases-index?tag=uc [Irritable Bowel Syndrome]https://fmt-japan.org/research-activities/fmt-cases-index?tag=ibs [Atopic Allergies]https://fmt-japan.org/research-activities/fmt-cases-index?tag=allergy [Constipation]https://fmt-japan.org/research-activities/fmt-cases-index?tag=constipation [ASD (Autism Spectrum Disorder)]https://fmt-japan.org/research-activities/fmt-cases-index?tag=asd [Other Diseases]https://fmt-japan.org/research-activities/fmt-cases-index?tag=others
November 02, 2024
12-year-old girl with autism spectrum disorder -Fecal microbiota transplant case report
Case presentation 12-year-old girl with autistic spectrum disorder summary A case of transplantation for autistic spectrum disorder. Improvement in bowel movements, sleep quality, and tantrums were observed, but not much change was seen in the hyperactivity aspect or impulsivity. Basic Information Patients :12-year-old girlAttending physician :Luke’s Ashiya ClinicMedical institution in charge of transplantation :Luke’s Ashiya […]
November 02, 2024
6-year-old boy with autism spectrum disorder -Fecal microbiota transplant case report
Case presentation 6-year-old boy with autistic spectrum disorder summary A case of transplantation for autism spectrum disorder (ASD). The patient has difficulty in understanding his surroundings and tends to be hyperactive. The main complaint was lack of concentration. No significant change was observed after transplantation. Basic Information Patients :6 year old boyAttending physician :Luke’s Ashiya […]